Did you know over 200 million people worldwide have osteoporosis? Research shows one in three women and one in five men over 50 will face a fracture because of this disease. This fact highlights how serious low bone density can be. Osteoporosis is common, increasing fracture risks and leading to health problems and less quality of life.
This article will cover the basics of osteoporosis. We will look at its causes, signs, and ways to handle it. Knowing about osteoporosis is vital for those at risk. It helps keep bones healthy and prevents problems from bone loss.
Key Takeaways
- Osteoporosis affects millions worldwide and is a major public health issue.
- It can increase the chance of fractures and long-term health issues.
- It’s important to understand the causes and how to prevent bone loss.
- Stats show a worrying trend among older people and fracture cases.
- Early detection and management greatly help improve bone health.
Understanding Osteoporosis and Its Prevalence
Bone health is key to how well we feel overall. It helps our body stand strong and function right. As we get older, our bones might get weaker. This raises the chance of getting osteoporosis. We can keep our bones healthy with good food, moving our body, and making better lifestyle choices.
Overview of Bone Health
Keeping bones strong is really important, especially as we get older. Osteoporosis becomes more common in older people. It can cause more breaks and disabilities. Changes in hormones and your genes can raise your risk. Eating foods with enough calcium and vitamin D is one way to support bone health.
Statistics on Osteoporosis Incidence
Many people around the world have osteoporosis. Over 200 million people are living with it today. In the U.S., 1 in 3 women and 1 in 5 men over 50 might break a bone because of it. About 30% of women in Europe and the U.S. have osteoporosis.
Getting older makes you more likely to develop osteoporosis. After 50, the risk of breaking a hip is 3.5% for men and 14.6% for women. This issue is more common in Caucasians, older adults, and women. Here are some important statistics about osteoporosis:
| Statistic | Percentage |
|---|---|
| Global Prevalence | 18.3% |
| Prevalence in Women | 23.1% |
| Prevalence in Men | 11.7% |
| Women Aged 50 or Older (U.S.) | 30% |
| Men Aged 50 or Older (U.S.) | 20% |
| Prevalence in Various Regions | 24.7% in India (Men and Women) |
Every year, there are over 8.9 million fractures because of osteoporosis. Knowing about this and how it affects bone health is very important. The new research emphasizes the need for ways to prevent and find osteoporosis early.
Introduction: Osteoporosis
Osteoporosis makes bones fragile and more likely to break. We need to understand what it is and its effects. Many do not know they have it until a bone breaks. This shows why we must know more about it and how to prevent it.
Definition and Medical Insights
Osteoporosis definition means bones get less dense and weaker. This puts older adults at a higher risk of breaking bones. Most people don’t know they have osteoporosis until they break a bone. Every year, about 1.5 million breaks in the U.S. are because of this. Half of women and a quarter of men over 50 will likely break a bone due to osteoporosis.
Bone Thinning Disease Explained
Osteopenia is when you lose some bone mass. Osteoporosis is when you lose a lot. Bones get porous and weak. Women especially, after 45, face a high risk. Twenty percent get osteoporosis, and thirty percent have low bone mass. The risk gets higher after 65. It also leads to high healthcare costs, affecting society.
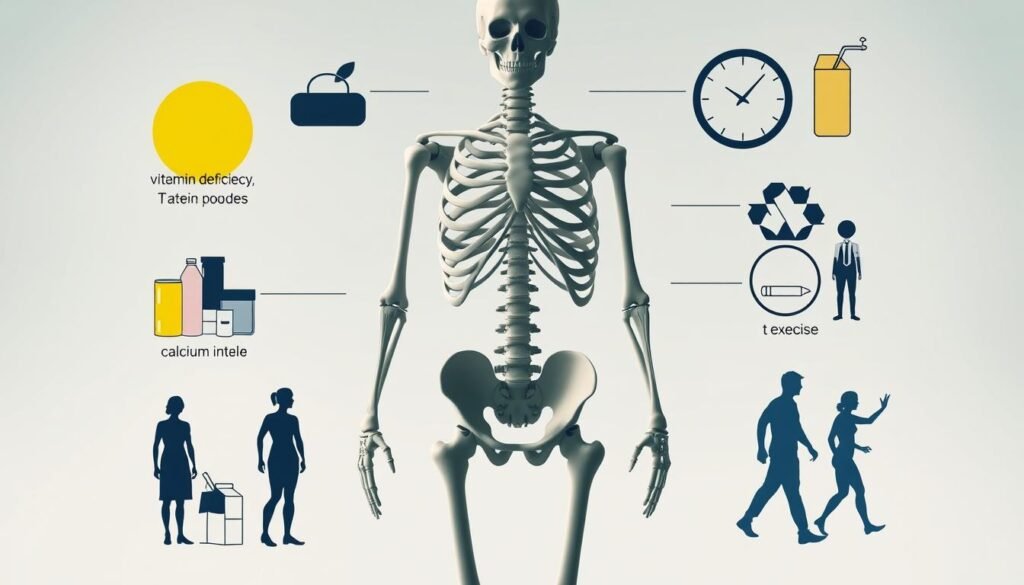
Causes of Bone Loss and Low Bone Density
It’s really important to understand what makes bone density go down to fight osteoporosis. Many things can make bones weaker, especially as people get older. Knowing these causes helps with better prevention and care.
Age-Related Factors
As people age, bones naturally start to lose mass. Studies show that after 50, men and women lose 1% to 3% of their bone mass every year. This loss gets worse over time, so it is important to keep an eye on bone health as one gets older.
Hormonal Changes and Osteoporosis
Hormones play a big part in the risk of osteoporosis. For women, losing estrogen after menopause makes bone loss faster. Men are less impacted but still face bone loss with lower testosterone. These hormonal changes make fractures more likely.
Impact of Medications and Lifestyle Choices
Some medications and lifestyle choices can also increase the risk of osteoporosis. Certain drugs may lower bone density. Bad habits like drinking too much alcohol and smoking are harmful too. Not being active enough is bad for bones, highlighting the need for regular exercise to keep bones strong.
| Factor | Description | Impact on Bone Density |
|---|---|---|
| Age | Natural decline post-50 | 1-3% loss annually |
| Hormonal Changes | Decreased estrogen and testosterone | Accelerated bone loss |
| Medications | Certain drugs affecting bone health | Increased risk of fractures |
| Lifestyle Choices | Alcohol consumption, smoking, inactivity | Reduces bone density and health |
Key Risk Factors for Osteoporosis
Learning about osteoporosis risk factors helps people avoid this bone condition. Things like genetics, what you eat, your gender, and where you come from play a part. Knowing them helps take early steps and make smart choices for your health.
Genetic Predisposition
If your family has a history of osteoporosis, you might face a higher risk too. Having relatives who had fractures makes your own risk greater. It’s crucial to get checked early and manage your health wisely.
Dietary Deficiencies: Calcium and Vitamin D
For strong bones, calcium and vitamin D are vital. You need about 1,200 mg of calcium daily, and vitamin D helps your body use that calcium. Not getting enough can lead to bone problems and fractures later in life.
Gender and Ethnicity Considerations
Women are more likely to get osteoporosis than men, especially after menopause. Ethnic background matters too, with Caucasians and Asians having a bigger chance of thin bones. Knowing this can guide prevention efforts for those most at risk.
| Risk Factor | Impact on Osteoporosis Risk |
|---|---|
| Genetic Predisposition | Higher risk if family history exists |
| Calcium Deficiency | Weakens bones, leads to fractures |
| Vitamin D Deficiency | Impedes calcium absorption, increases fracture risk |
| Gender | Higher prevalence in women, especially post-menopause |
| Ethnicity | Caucasians and Asians at increased risk for lower bone density |
For more insights on osteoporosis and how to manage your risk, visit the National Institutes of Health. Being informed is the first step to better health for those at risk.
Recognizing Symptoms of Osteoporosis
It’s key to know the signs of osteoporosis early on. This quiet disease often doesn’t show symptoms, making it hard to spot before it causes major damage. Spotting osteoporosis symptoms early can lead to quick action and better health.
Silent Nature of the Disease
Osteoporosis is called a “silent disease” because symptoms often don’t appear until a fracture happens. Many people don’t see any signs, which lets the disease get worse unseen. Around 21.2% of women and 6.3% of men over 50 across the globe are affected. Most won’t know they have it until they incur a serious injury.
Common Signs and Symptoms
Spotting osteoporosis symptoms isn’t easy due to their subtle start. Yet, some signs could hint at bone health going downhill. Look out for these symptoms:
- Sudden back pain, often because of a fracture
- Getting shorter over time
- Stooped posture, usually from spinal compression fractures
- Breaking bones easily, like after a small bump
Putting early spotting and prevention first is crucial for managing this disease. This ensures healthy bones for a long time.
Diagnosing Osteoporosis
To diagnose osteoporosis, doctors use several methods to check bone health and fracture risks. Early diagnosis means better management and treatment, especially for those at higher risk. Bone density tests are key in this process.
Bone Density Tests and Importance
The main way to diagnose osteoporosis is through dual-energy X-ray absorptiometry (DXA). This test, which is not invasive, measures how dense the bones are. People over 65 or with certain risks should get tested regularly. However, not enough older adults are getting this important test.
Understanding T-scores and Z-scores
Bone density test results come as T-scores and Z-scores. These scores give clues about a person’s bone health. A T-score shows how your bone density compares to a healthy young adult’s average. If your score is -2.5 or less, it means osteoporosis. Z-scores compare your bone density to people your age and gender. This helps understand bone health in your own group. Interestingly, not everyone with hip fractures has very low T-scores, showing fractures can happen without severely low bone density.

| Bone Density Test Result | Interpretation | Fracture Risk Implications |
|---|---|---|
| T-score ≤ -2.5 | Osteoporosis | High risk of fractures |
| T-score between -1.0 and -2.5 | Osteopenia (low bone mass) | Moderate risk of fractures |
| T-score > -1.0 | Normal Bone Density | Low risk of fractures |
Knowing how to diagnose osteoporosis well helps doctors take care of it better. This can mean less risk of fractures for patients. Finding it early using the right tests means people can stay healthier.
Management and Treatment Options
To manage osteoporosis effectively, a combination of medications and supplements is vital. These treatments help improve bone health. They aim to reduce bone loss, boost bone density, and cut the risk of fractures.
Medication: Types and Benefits
Many medicines help treat osteoporosis. They include anti-resorptive, bone-forming, and dual-acting types. Doctors often prescribe:
- Bisphosphonates: These decrease bone loss.
- Denosumab: A monoclonal antibody slowing down bone loss.
- Selective Estrogen Receptor Modulators (SERMs): They act like estrogen to keep bones strong.
- Parathyroid Hormone (PTH): It helps create new bone.
- Romosozumab: This new medicine does both–increases bone formation and lowers resorption.
Choosing the right medication depends on several factors like age, gender, and fracture history. Studies show that denosumab is cost-effective, particularly in older men. Hormone replacement therapy can reduce fractures in post-menopausal women.
Role of Supplements in Bone Health
Nutrition is key in osteoporosis management. Calcium and vitamin D are crucial for bone health. They’re particularly important for those who can’t get enough through their diet. Doctors often recommend:
- Calcium Supplements: These ensure you get enough calcium.
- Vitamin D Supplements: They help your body use calcium better and support bone growth.
Keeping calcium and vitamin D levels high is essential to prevent bone loss. It’s important to get regular screenings and discuss osteoporosis treatments with healthcare professionals.
| Medication Type | Mechanism | Examples |
|---|---|---|
| Anti-resorptive | Reduces bone resorption | Bisphosphonates, Denosumab |
| Bone-forming | Stimulates new bone growth | Parathyroid Hormone |
| Dual-acting | Both increases formation & decreases resorption | Romosozumab |
Preventing Osteoporosis: Lifestyle Changes
Taking early steps is key to stop osteoporosis. Making lifestyle changes greatly boosts bone health and lowers fracture risks. Adopting good strategies like doing weight-bearing exercises and eating well helps maintain bone density.
Importance of Weight-Bearing Exercises
Exercises like walking, jogging, and lifting weights are crucial for strong bones. These actions make bones stronger by causing them to rebuild. Doing these exercises often can make bones denser, a must to avoid osteoporosis.
Nutrition and Dietary Strategies
Eating foods full of calcium and vitamin D is vital for healthy bones. Dairy, green veggies, and foods with added nutrients are important to eat every day. Good nutrition helps keep bones strong, helping to stop osteoporosis.
Reducing Fall Risks at Home
Keeping your home safe is essential to prevent bone breaks from falls. Taking steps to lower the chance of falling is key for people with fragile bones. Making your home safer, like better lights, less clutter, and securing carpets, helps prevent accidents.

Implications of Osteoporosis on Health
Osteoporosis makes it hard on health, mainly because it increases fracture risks. Knowing about these fracture risks is key to understand how much osteoporosis affects people. In the U.S., over 54 million have it. This raises the chances of breaking bones like the hip, spine, and wrist, which leads to serious health problems.
Fracture Risks and Their Consequences
The facts on osteoporosis are quite shocking. About half of women and a quarter of men over 50 will break a bone due to osteoporosis. These fractures are not just painful; they lead to huge costs – $19 billion each year. By 2025, the fractures could double, costing more than $25 billion. Elderly folks who break a hip are at a 20% higher risk of dying within a year. This shows why we need to take the osteoporosis impact seriously for public health.
Impact on Quality of Life
Osteoporosis also hurts the way people live. Fear of breaking a bone can cause folks to move less and lose their independence. This hurts their quality of life. It’s not just physical; mental well-being also drops. A lot of those with osteoporosis feel depressed. This mental strain makes it tougher to deal with physical limits from fractures. It also puts more pressure on those who care for them and the health systems. We need good prevention and treatment plans. They can make life better and lower costs from osteoporosis issues. For more on this, visit this source.
Conclusion
Understanding osteoporosis is key to stopping it before it starts. As we get older, keeping bones strong through good lifestyle choices is crucial. Simple changes in what we eat and how much we move can greatly cut osteoporosis risk.
Eating foods rich in calcium and vitamin D is important. So is doing exercises that make you bear weight. We also need to teach people more about stopping osteoporosis. Many don’t know their risk until it’s too late.
We must keep pushing to better the lives of those at risk for osteoporosis. The numbers on fractures and health problems are too high to ignore. With better knowledge and life choices, we can fight the dangers of this disease. For more insights on osteoporosis, check out resources from the National Institutes of Health.